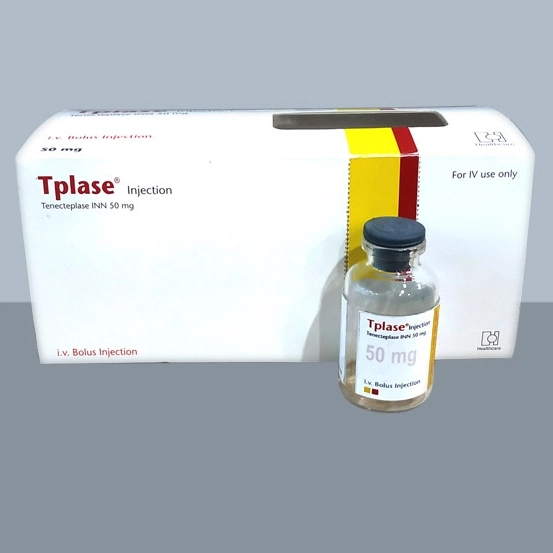
50 mg vial:
৳ 55,000.00
Indications
Tplase is indicated in Acute phase of myocardial infarction (AMI).
* রেজিস্টার্ড চিকিৎসকের পরামর্শ মোতাবেক ঔষধ সেবন করুন
Description
Tplase is a tissue plasminogen activator (tPA) produced by recombinant DNA technology using an established mammalian cell line (Chinese Hamster Ovary cells). Tplase is a 527 amino acid glycoprotein developed by introducing the following modifications to the complementary DNA (cDNA) for natural human tPA: a substitution of threonine 103 with asparagine, and a substitution of asparagine 117 with glutamine, both within the kringle 1 domain, and a tetra-alanine substitution at amino acids 296–299 in the protease domain. Tenectaplase is a sterile, white to off-white, lyophilized powder for single intravenous (IV) bolus administration after reconstitution with Sterile Water for Injection (SWFI), USP. Each vial of Tenectaplase nominally contains 52.5 mg Tplase, 0.55 g L-arginine, 0.17 g phosphoric acid, and 4.3 mg polysorbate 20, which includes a 5% overfill. Each vial will deliver 50 mg of Tplase.
Pharmacology
Tenecteplase is a recombinant fibrin-specific plasminogen activator that is derived from native t-PA by modifications at three sites of the protein structure. It binds to the fibrin component of the thrombus (blood clot) and selectively converts thrombus-bound plasminogen to plasmin, which degrades the fibrin matrix of the thrombus. Tenecteplase has a higher fibrin specificity and greater resistance to inactivation by its endogenous inhibitor (PAI-1) compared to native t-PA. Tenecteplase binds to fibrin rich clots via the fibronectin finger-like domain and the Kringle 2 domain. The protease domain then cleaves the Arg/Val bond in plasminogen to form plasmin. Plasmin in turn degrades the fibrin matrix of the thrombus, thereby exerting its thrombolytic action.
Dosage
Tenecteplase is for intravenous administration only. The recommended total dose should not exceed 50 mg and is based upon patient weight. A single bolus dose should be administered over 5 seconds based on patient weight. Treatment should be initiated as soon as possible after the onset of AMI symptoms.
- Patient Weight <60 kg: 30 mg Tenecteplase
- Patient Weight ≥60 to <70 kg: 35 mg Tenecteplase
- Patient Weight ≥70 to <80 kg: 40 mg Tenecteplase
- Patient Weight ≥80 to <90 kg: 45 mg Tenecteplase
- Patient Weight ≥90 kg: 50 mg Tenecteplase
* রেজিস্টার্ড চিকিৎসকের পরামর্শ মোতাবেক ঔষধ সেবন করুন
Administration
Readministration of plasminogen activators, including Tenecteplase, to patients who have received prior plasminogen activator therapy has not been systematically studied. Three of 487 patients tested for antibody formation to Tenecteplase had a positive antibody titer at 30 days. The data reflect the percentage of patients whose test results were considered positive for antibodies to Tenecteplase in a radioimmunoprecipitation assay, and are highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody positivity in an assay may be influenced by several factors including sample handling, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to Tenecteplase with the incidence of antibodies to other products may be misleading. Although sustained antibody formation in patients receiving one dose of Tenecteplase has not been documented, readministration should be undertaken with caution.
* রেজিস্টার্ড চিকিৎসকের পরামর্শ মোতাবেক ঔষধ সেবন করুন
Interaction
No formal interaction studies with Tplase and medicinal products commonly administered in patients with AMI have been performed. Medicinal products that affect coagulation or those that alter platelet function may increase the risk of bleeding prior to, during or after Tplase therapy.
Contraindications
Active internal bleeding; history of cerebrovascular accident; intracranial or intraspinal surgery, or trauma within 2 months; intracranial neoplasm, arteriovenous malformation, or aneurysm; known bleeding diathesis; and severe uncontrolled hypertension.
Side Effects
The most frequent adverse reaction associated with Tplase is bleeding. If serious bleeding occurs, concomitant heparin and antiplatelet therapy should be discontinued. Death or permanent disability can occur in patients who experience stroke or serious bleeding episodes.For Tplase-treated patients in ASSENT-2, the incidence of intracranial hemorrhage was 0.9% and any stroke was 1.8%. The incidence of all strokes, including intracranial bleeding, increases with increasing age. Non-intracranial major bleeding and the need for blood transfusions were lower in patients treated with Tplase.Types of major bleeding reported in 1% or more of the patients were hematoma (1.7%) and gastrointestinal tract (1%). Types of major bleeding reported in less than 1% of the patients were urinary tract, puncture site (including cardiac catheterization site), retroperitoneal, respiratory tract, and unspecified. Types of minor bleeding reported in 1% or more of the patients were hematoma (12.3%), urinary tract (3.7%), puncture site (including cardiac catheterization site) (3.6%), pharyngeal (3.1%), gastrointestinal tract (1.9%), epistaxis (1.5%), and unspecified (1.3%).
The following adverse reactions have been reported among patients receiving Tplase in clinical trials. These reactions are frequent sequelae of the underlying disease, and the effect of Tplase on the incidence of these events is unknown. These events include cardiogenic shock, arrhythmias, atrioventricular block, pulmonary edema, heart failure, cardiac arrest, recurrent myocardial ischemia, myocardial reinfarction, myocardial rupture, cardiac tamponade, pericarditis, pericardial effusion, mitral regurgitation, thrombosis, embolism, and electromechanical dissociation. These events can be life-threatening and may lead to death. Nausea and/or vomiting, hypotension, and fever have also been reported.
The following adverse reactions have been reported among patients receiving Tplase in clinical trials. These reactions are frequent sequelae of the underlying disease, and the effect of Tplase on the incidence of these events is unknown. These events include cardiogenic shock, arrhythmias, atrioventricular block, pulmonary edema, heart failure, cardiac arrest, recurrent myocardial ischemia, myocardial reinfarction, myocardial rupture, cardiac tamponade, pericarditis, pericardial effusion, mitral regurgitation, thrombosis, embolism, and electromechanical dissociation. These events can be life-threatening and may lead to death. Nausea and/or vomiting, hypotension, and fever have also been reported.
Pregnancy & Lactation
The benefit of treatment must be evaluated against the potential risks in case of myocardial infarction during pregnancy. It is not known if tenecteplase is excreted into breast milk. It is not known if Tenecteplase is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when tenecteplase is administered to a nursing woman.
Precautions & Warnings
General: Standard management of myocardial infarction should be implemented concomitantly with Tplase treatment. Arterial and venous punctures should be minimized. Noncompressible arterial puncture must be avoided and internal jugular and subclavian venous punctures should be avoided to minimize bleeding from the noncompressible sites. In the event of serious bleeding, heparin and antiplatelet agents should be discontinued immediately. Heparin effects can be reversed by protamine.
Hypersensitivity: Hypersensitivity, including urticarial / anaphylactic reactions, have been reported after administration of Tplase (e.g., anaphylaxis, angioedema, laryngeal edema, rash, and urticaria). Monitor patients treated with Tplase during and for several hours after infusion. If symptoms of hypersensitivity occur, appropriate therapy should be initiated.
Hypersensitivity: Hypersensitivity, including urticarial / anaphylactic reactions, have been reported after administration of Tplase (e.g., anaphylaxis, angioedema, laryngeal edema, rash, and urticaria). Monitor patients treated with Tplase during and for several hours after infusion. If symptoms of hypersensitivity occur, appropriate therapy should be initiated.
Use in Special Populations
Pediatric Use: The safety and effectiveness of Tplase in pediatric patients have not been established.
Geriatric Use: Of the patients in ASSENT-2 who received Tplase, 4,958 (59%) were under the age of 65; 2,256 (27%) were between the ages of 65 and 74; and 1,244 (15%) were 75 and over. The 30-day mortality rates by age were 2.5% in patients under the age of 65, 8.5% in patients between the ages of 65 and 74, and 16.2% in patients age 75 and over. The ICH rates were 0.4% in patients under the age of 65, 1.6% in patients between the ages of 65 and 74, and 1.7% in patients age 75 and over. The rates of any stroke were 1.0% in patients under the age of 65, 2.9% in patients between the ages of 65 and 74, and 3.0% in patients age 75 and over. Major bleeding rates, defined as bleeding requiring blood transfusion or leading to hemodynamic compromise, were 3.1% in patients under the age of 65, 6.4% in patients between the ages of 65 and 74, and 7.7% in patients age 75 and over. In elderly patients, the benefits of Tplase on mortality should be carefully weighed against the risk of increased adverse events, including bleeding.
Geriatric Use: Of the patients in ASSENT-2 who received Tplase, 4,958 (59%) were under the age of 65; 2,256 (27%) were between the ages of 65 and 74; and 1,244 (15%) were 75 and over. The 30-day mortality rates by age were 2.5% in patients under the age of 65, 8.5% in patients between the ages of 65 and 74, and 16.2% in patients age 75 and over. The ICH rates were 0.4% in patients under the age of 65, 1.6% in patients between the ages of 65 and 74, and 1.7% in patients age 75 and over. The rates of any stroke were 1.0% in patients under the age of 65, 2.9% in patients between the ages of 65 and 74, and 3.0% in patients age 75 and over. Major bleeding rates, defined as bleeding requiring blood transfusion or leading to hemodynamic compromise, were 3.1% in patients under the age of 65, 6.4% in patients between the ages of 65 and 74, and 7.7% in patients age 75 and over. In elderly patients, the benefits of Tplase on mortality should be carefully weighed against the risk of increased adverse events, including bleeding.
Overdose Effects
In the event of overdose there may be an increased risk of bleeding. In case of severe prolonged bleeding substitution therapy may be considered (plasma, platelets).
Therapeutic Class
Fibrinolytics (Thrombolytics)
Reconstitution
Remove the syringe from the supplied JMI complimentary pouch and aseptically withdraw 10 mL of Sterile Water for Injection(SWFI), USP, from the supplied diluent vial. Do not use Bacteriostatic Water for Injection, USP.
Inject the entire contents of the syringe (10 mL) into the Tplase vial directing the diluent stream into the powder. Slight foaming upon reconstitution is not unusual; any large bubbles will dissipate if the product is allowed to stand undisturbed for several minutes.
Gently swirl until contents are completely dissolved. DO NOT SHAKE. The reconstituted preparation results in a colorless to pale yellow transparent solution containing Tplase at 5 mg/mL at a pH approximately 7.30-7.50.
Determine the appropriate dose of Tplase and withdraw this volume (in milliliters) from the reconstituted vial with the syringe. Any unused solution should be discarded.
Once the appropriate dose of Tplase is drawn into the syringe, stand the shield vertically on a flat surface.
Inject the entire contents of the syringe (10 mL) into the Tplase vial directing the diluent stream into the powder. Slight foaming upon reconstitution is not unusual; any large bubbles will dissipate if the product is allowed to stand undisturbed for several minutes.
Gently swirl until contents are completely dissolved. DO NOT SHAKE. The reconstituted preparation results in a colorless to pale yellow transparent solution containing Tplase at 5 mg/mL at a pH approximately 7.30-7.50.
Determine the appropriate dose of Tplase and withdraw this volume (in milliliters) from the reconstituted vial with the syringe. Any unused solution should be discarded.
Once the appropriate dose of Tplase is drawn into the syringe, stand the shield vertically on a flat surface.
Storage Conditions
Store lyophilized Tplase at temperature not exceeding 30°C or under refrigerator 2-8°C. Keep out of reach of children.