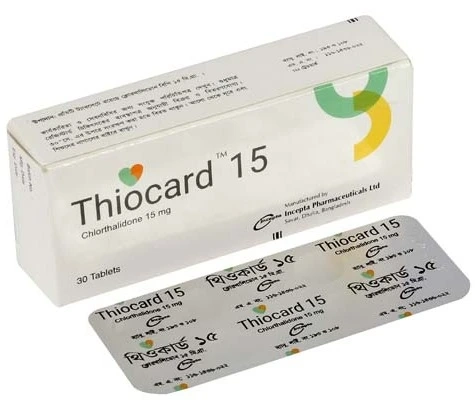
Unit Price:
৳ 4.00
(3 x 10: ৳ 120.00)
Strip Price:
৳ 40.00
Also available as:
Indications
Thiocard is indicated in the management of hypertension. Thiocard is indicated as adjunctive therapy in edema associated with congestive heart failure, hepatic cirrhosis and corticosteroid and estrogen therapy.
* রেজিস্টার্ড চিকিৎসকের পরামর্শ মোতাবেক ঔষধ সেবন করুন
Pharmacology
Chlorthalidone is a thiazide-type Diuretic- Antihypertensive, used for the treatment of hypertension. It may be used alone or in association with other antihypertensive agents. Chlortalidone is also indicated for adjunctive therapy of edema associated with: renal disease; congestive heart failure of mild to moderate degree (functional class II, Ill), when glomerular filtration rate is greater than 30 ml/min; ascites due to cirrhosis of the liver in stable patients; estrogen therapy; corticosteroid therapy.
Chlorthalidone inhibits the reabsorption of sodium and chloride in the distal renal tubule thus promoting water loss. The higher urine volume increases potassium loss. Little information is available on the absorption of the drug. Its long elimination half-life and clinical experience place it as a long-acting thiazide derivative. The longer-acting agents appear to cause increased potassium loss.
Although a mild diuretic, its combination with loop diuretics is particularly potent because the latter presents much more sodium chloride to the distal tubule.
The blood pressure lowering effects are initially due to volume reduction but the persisting effect includes other undetermined mechanisms that reduce peripheral resistance. A high salt intake reverses its antihypertensive effect.
The major portion of an absorbed dose of Chlorthalidone is excreted by the kidneys with an elimination half life averaging 50 hours. Metabolism and hepatic excretion into the bile constitute a minor way of elimination. Within 120 hours, about 70% of the dose is excreted in the urine and in the feces, mainly in an unchanged form.
Chlorthalidone inhibits the reabsorption of sodium and chloride in the distal renal tubule thus promoting water loss. The higher urine volume increases potassium loss. Little information is available on the absorption of the drug. Its long elimination half-life and clinical experience place it as a long-acting thiazide derivative. The longer-acting agents appear to cause increased potassium loss.
Although a mild diuretic, its combination with loop diuretics is particularly potent because the latter presents much more sodium chloride to the distal tubule.
The blood pressure lowering effects are initially due to volume reduction but the persisting effect includes other undetermined mechanisms that reduce peripheral resistance. A high salt intake reverses its antihypertensive effect.
The major portion of an absorbed dose of Chlorthalidone is excreted by the kidneys with an elimination half life averaging 50 hours. Metabolism and hepatic excretion into the bile constitute a minor way of elimination. Within 120 hours, about 70% of the dose is excreted in the urine and in the feces, mainly in an unchanged form.
Dosage & Administration
Therapy should be initiated with the lowest possible dose, and be titrated thereafter to gain maximum therapeutic benefit while keeping side effects to a minimum (e.g. determine the minimum effective maintenance dose for each patient). A single dose daily or every other day is given in the morning with food is recommended.
Hypertension: Usual adult dose is 25 to 50 mg daily. The clinically useful dosage range is 12.5 to 50 mg daily. Doses greater than 50 mg per day increase metabolic complications and are rarely of therapeutic benefit. For a given dose, the full effect is reached after 3 to 4 weeks. If the decrease in blood pressure obtained using doses of 25 or 50 mg/day proves inadequate, combined treatment with other antihypertensive drugs (such as beta-blockers and ACE inhibitors) is recommended. When adding an ACE inhibitor, Chlorthalidone is to be reduced or discontinued.
Edema of Specific Origin: The lowest effective dose is to be identified by titration. Maintenance doses should not exceed 50 mg/day and should be administered over limited periods only. The dosage should be individually adapted to the clinical picture and patient response. For long-term therapy, the lowest possible dosage sufficient to maintain an optimal effect should be employed; this applies particularly to elderly patients.
The therapeutic effect of Chlorthalidone occurs even without salt restriction and is well sustained during continued use.
The elderly: This is a suitable drug for treating hypertension in the elderly, in particular systolic hypertension. Dose of 50 mg daily, or less, should be used to avoid hypovolemia and hypokalemia.
Hypertension: Usual adult dose is 25 to 50 mg daily. The clinically useful dosage range is 12.5 to 50 mg daily. Doses greater than 50 mg per day increase metabolic complications and are rarely of therapeutic benefit. For a given dose, the full effect is reached after 3 to 4 weeks. If the decrease in blood pressure obtained using doses of 25 or 50 mg/day proves inadequate, combined treatment with other antihypertensive drugs (such as beta-blockers and ACE inhibitors) is recommended. When adding an ACE inhibitor, Chlorthalidone is to be reduced or discontinued.
Edema of Specific Origin: The lowest effective dose is to be identified by titration. Maintenance doses should not exceed 50 mg/day and should be administered over limited periods only. The dosage should be individually adapted to the clinical picture and patient response. For long-term therapy, the lowest possible dosage sufficient to maintain an optimal effect should be employed; this applies particularly to elderly patients.
The therapeutic effect of Chlorthalidone occurs even without salt restriction and is well sustained during continued use.
The elderly: This is a suitable drug for treating hypertension in the elderly, in particular systolic hypertension. Dose of 50 mg daily, or less, should be used to avoid hypovolemia and hypokalemia.
* রেজিস্টার্ড চিকিৎসকের পরামর্শ মোতাবেক ঔষধ সেবন করুন
Interaction
Other interactions: Patients with Special Diseases and Conditions in patients with impaired hepatic function or progressive liver disease, caution should be exercised since even minor alterations in fluid and electrolyte balance or of serum ammonia may precipitate hepatic coma. Treatment with thiazide diuretics should be initiated cautiously in postsympathectomy patients since the antihypertensive effects may be enhanced. A cautious dosage schedule should be adopted in patients with severe coronary or cerebral ateriosderosis.
Drug Interactions-
Antihypertensive Agents: Diuretics potentiate the action of curare derivatives and antihypertensive agents (e.g. guanethidine, methyldopa, beta-blockers, vasodilators, calcium antagonists, ACE inhibitors).
Digitalis: Thiazide-induced hypokalemia or hypomagnesemia may increase the likelihood of digitalis-induced cardiac arrhythmias (see also Precautions).
Corticosteroids: The hypokalemic effects of diuretics may be increased by corticosteroids, ACTH and amphotericin. Insulin and Oral Antidiabetic Agents: It may be necessary to adjust the dosage of insulin or oral antidiabetic agents in response to changes in glucose tolerance that Thiocard may produce.
NSAIDs: Concomitant administration of certain NSAIDs (e.g. indomethacin) may weaken the diuretic and antihypertensive activity of thiazides, and there have been isolated reports of a deterioration of renal function in predisposed patients.
Curare Derivatives and Ganglionic Blocking Agents: Thiazides may increase responsiveness to curare derivatives and ganglionic blocking agents.
Allopurinol: Co-administration of thiazide diuretics may increase the incidence of hypersensitivity reactions to allopurinol.
Amantadine: Co-administration of thiazide diuretics may increase the risk of adverse effects from amantadine.
Antineoplastic Agents (e.g. cyclophosphamide, methotrexate): Concomitant use of thiazide diuretics may reduce renal excretion of cytotoxic agents and enhance the myelo suppressive effects. Anticholinergics (e.g. atropine, biperiden): The bioavailability of thiazide-type diuretics may be increased by anticholinergic agents, apparently due to a decrease in gastrointestinal motility and rate of gastric emptying.
Cholestyramine: Absorption of thiazide diuretics is decreased by cholestyramine, therefore a decrease in pharmacological effect may be expected.
Vitamin D: Concomitant use of thiazide diuretics may decrease urinary excretion of calcium, and co-administration of Vitamin D may potentiate the increase in serum calcium.
Cyclosporin: Concomitant treatment with diuretics may increase the risk of hyperuricemia and gout-type complications.
Calcium Salts: Concomitant use of thiazide-type diuretics may cause hypercalcemia by increasing tubular calcium reabsorption.
Diazoxide: Thiazide diuretics may enhance the hyperglycemic effect of diazoxide.
Drug Interactions-
Antihypertensive Agents: Diuretics potentiate the action of curare derivatives and antihypertensive agents (e.g. guanethidine, methyldopa, beta-blockers, vasodilators, calcium antagonists, ACE inhibitors).
Digitalis: Thiazide-induced hypokalemia or hypomagnesemia may increase the likelihood of digitalis-induced cardiac arrhythmias (see also Precautions).
Corticosteroids: The hypokalemic effects of diuretics may be increased by corticosteroids, ACTH and amphotericin. Insulin and Oral Antidiabetic Agents: It may be necessary to adjust the dosage of insulin or oral antidiabetic agents in response to changes in glucose tolerance that Thiocard may produce.
NSAIDs: Concomitant administration of certain NSAIDs (e.g. indomethacin) may weaken the diuretic and antihypertensive activity of thiazides, and there have been isolated reports of a deterioration of renal function in predisposed patients.
Curare Derivatives and Ganglionic Blocking Agents: Thiazides may increase responsiveness to curare derivatives and ganglionic blocking agents.
Allopurinol: Co-administration of thiazide diuretics may increase the incidence of hypersensitivity reactions to allopurinol.
Amantadine: Co-administration of thiazide diuretics may increase the risk of adverse effects from amantadine.
Antineoplastic Agents (e.g. cyclophosphamide, methotrexate): Concomitant use of thiazide diuretics may reduce renal excretion of cytotoxic agents and enhance the myelo suppressive effects. Anticholinergics (e.g. atropine, biperiden): The bioavailability of thiazide-type diuretics may be increased by anticholinergic agents, apparently due to a decrease in gastrointestinal motility and rate of gastric emptying.
Cholestyramine: Absorption of thiazide diuretics is decreased by cholestyramine, therefore a decrease in pharmacological effect may be expected.
Vitamin D: Concomitant use of thiazide diuretics may decrease urinary excretion of calcium, and co-administration of Vitamin D may potentiate the increase in serum calcium.
Cyclosporin: Concomitant treatment with diuretics may increase the risk of hyperuricemia and gout-type complications.
Calcium Salts: Concomitant use of thiazide-type diuretics may cause hypercalcemia by increasing tubular calcium reabsorption.
Diazoxide: Thiazide diuretics may enhance the hyperglycemic effect of diazoxide.
Contraindications
Anuria, severe renal failure (creatinine clearance lower than 30 mL/min), severe hepatic failure, refractory hypokalemia or conditions involving enhanced potassium loss, hyponatremia, hypercalcemia, symptomatic hyperuricemia (history of gout or uric acid calculi). Hypersensitivity or suspected hypersensitivity to Chlorthalidone and other sulfonamide derivatives or their excipients.
Should be used with caution in patients with renal disease or with impaired hepatic function. Because of the possibility of progression of renal damage, periodic determination of the BUN and serum creatinine are indicated. Should there be an elevation of either parameter, treatment should be discontinued. Like thiazides, Chlorthalidone may lose its diuretic efficacy when glomerular filtration rate drops below 30 mL/min, a point at which treatment with loop diuretics may be more appropriate.
Electrolytes: As with thiazide diuretics, kaluresis induced by Chlorthalidone is dose dependent, and there is inter-individual variability in magnitude. With 25 mg/day, serum potassium concentration decreases average 0.5 mmol/L. If chronic treatment is contemplated, serum potassium concentrations should be determined initially, and then 3 to 4 weeks later. If thereafter, potassium balance is not disturbed further, concentrations should be assessed every 4 to 6 months. Conditions that may alter potassium balance include: vomiting, diarrhea, malnutrition, change in renal function (e.g. nephrosis), liver cirrhosis, hyperaldosteronism, or concomitant use of corticosteroids or ACTH. Titrated co-administration of an oral potassium salt (e.g. KCI) may be considered in patients: receiving digitalis; exhibiting signs of coronary heart disease, unless they are also receiving an ACE inhibitor; on high doses of a beta-adrenergic agonist; whose plasma potassium concentrations are less than 3.0 mmol/L.
Should be used with caution in patients with renal disease or with impaired hepatic function. Because of the possibility of progression of renal damage, periodic determination of the BUN and serum creatinine are indicated. Should there be an elevation of either parameter, treatment should be discontinued. Like thiazides, Chlorthalidone may lose its diuretic efficacy when glomerular filtration rate drops below 30 mL/min, a point at which treatment with loop diuretics may be more appropriate.
Electrolytes: As with thiazide diuretics, kaluresis induced by Chlorthalidone is dose dependent, and there is inter-individual variability in magnitude. With 25 mg/day, serum potassium concentration decreases average 0.5 mmol/L. If chronic treatment is contemplated, serum potassium concentrations should be determined initially, and then 3 to 4 weeks later. If thereafter, potassium balance is not disturbed further, concentrations should be assessed every 4 to 6 months. Conditions that may alter potassium balance include: vomiting, diarrhea, malnutrition, change in renal function (e.g. nephrosis), liver cirrhosis, hyperaldosteronism, or concomitant use of corticosteroids or ACTH. Titrated co-administration of an oral potassium salt (e.g. KCI) may be considered in patients: receiving digitalis; exhibiting signs of coronary heart disease, unless they are also receiving an ACE inhibitor; on high doses of a beta-adrenergic agonist; whose plasma potassium concentrations are less than 3.0 mmol/L.
Side Effects
Electrolytes and Metabolic Disorders: Frequent: mainly at higher doses, hypokalemia, hyperuricemia and rise in blood lipids. Occasional: hyponatremia, hypomagnesemia and hyperglycemia. Rare: hypercalcemia, glycosuria, worsening of diabetic metabolic state and gout.
Isolated cases: hypochloremic alkalosis.
Dermatology: Occasional: urticaria and other forms of skin rash. Rare: photosensitization.
Liver: Rare: Intrahepatic cholestasis or jaundice.
Cardiovascular: Occasional: postural hypotension, which may be aggravated by alcohol, anesthetics or sedatives. Rare: cardiac arrhythmias.
CNS: Occasional: dizziness, slow mentation and decreased reaction time.
Isolated cases: hypochloremic alkalosis.
Dermatology: Occasional: urticaria and other forms of skin rash. Rare: photosensitization.
Liver: Rare: Intrahepatic cholestasis or jaundice.
Cardiovascular: Occasional: postural hypotension, which may be aggravated by alcohol, anesthetics or sedatives. Rare: cardiac arrhythmias.
CNS: Occasional: dizziness, slow mentation and decreased reaction time.
Pregnancy & Lactation
Pregnancy: Chlorthalidone, like other diuretics, can cause placental hypoperfusion. Since they do not prevent or alter the course of EPH (edema, proteinuria, hypertension) preeclampsia, these drugs must not be used to treat hypertension in pregnant women. The use of Chlorthalidone for other indications (e.g. heart disease) in pregnancy should be avoided, particularly in the first trimester, unless the potential benefits outweigh the possible risks (e.g. when there are no safer altenatives).
Lactation: Chlorthalidone appears in breast milk, attaining concentrations of approximately 4% of maternal blood levels. Therefore use in nursing mothers should be avoided.
Lactation: Chlorthalidone appears in breast milk, attaining concentrations of approximately 4% of maternal blood levels. Therefore use in nursing mothers should be avoided.
Precautions & Warnings
Renal impairment: Thiocard dosage should be reduced in moderate renal failure - every 24 or 48 h - and should not be used in advanced renal failure.
Liver disease: There is a risk of precipitating hepatic encephalopathy in patients with liver cirrhosis and ascites.
Use in pregnancy: It is better to avoid Thiocard as it crosses the placenta.
Use in Lactation: In lactating mother, significant amount of Thiocard enter breast milk; like other long-acting thiazides, it can suppress lactation. Thiocard should not be prescribed for lactating mother.
Liver disease: There is a risk of precipitating hepatic encephalopathy in patients with liver cirrhosis and ascites.
Use in pregnancy: It is better to avoid Thiocard as it crosses the placenta.
Use in Lactation: In lactating mother, significant amount of Thiocard enter breast milk; like other long-acting thiazides, it can suppress lactation. Thiocard should not be prescribed for lactating mother.
Overdose Effects
Symptoms of acute overdosage include nausea, weakness, dizziness, and disturbances of electrolyte balance. The oral LD 50 of the drug in the mouse and the rat is more than 25,000 mg/kg body weight. The minimum lethal dose (MLD) in humans has not been established. There is no specific antidote, but gastric lavage is recommended, followed by supportive treatment. Where necessary, this may include intravenous dextrose-saline with potassium, administered with caution.
Therapeutic Class
Thiazide diuretics & related drugs
Storage Conditions
Keep below 30°C temperature, away from light & moisture. Keep out of the reach of children.