Unit Price:
৳ 11.00
(3 x 10: ৳ 330.00)
Strip Price:
৳ 110.00
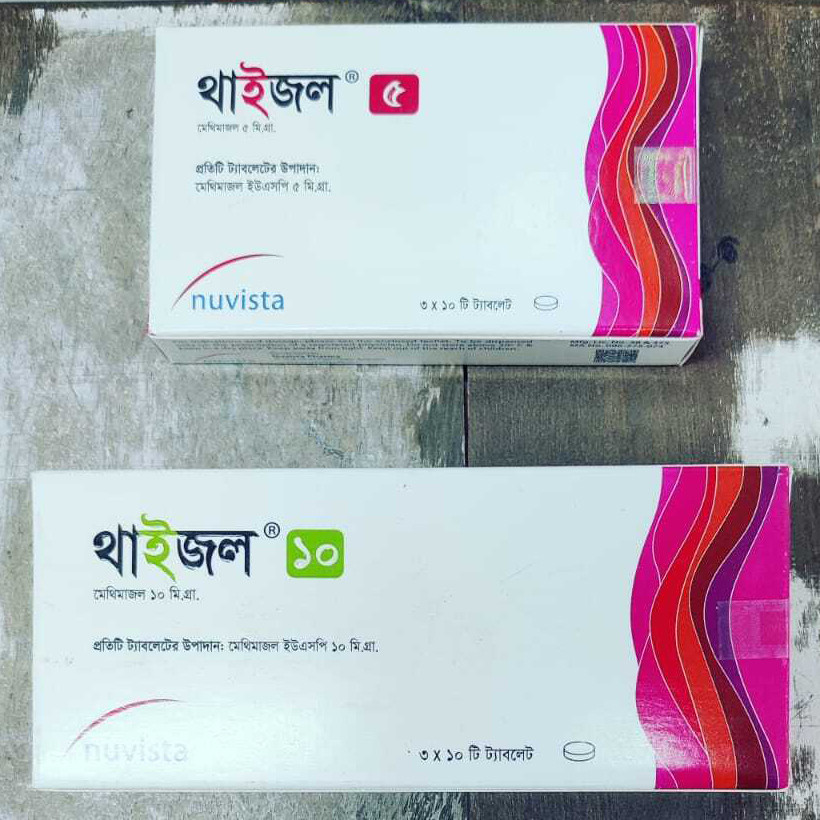
Also available as:
Indications
Thyzol is indicated:
- In patients with Graves' disease with hyperthyroidism or toxic multinodular goiter for whom surgery or radioactive iodine therapy is not an appropriate treatment option.
- To ameliorate symptoms of hyperthyroidism in preparation for thyroidectomy or radioactive iodine therapy.
* রেজিস্টার্ড চিকিৎসকের পরামর্শ মোতাবেক ঔষধ সেবন করুন
Pharmacology
Methimazole inhibits the synthesis of thyroid hormones and thus is effective in the treatment of hyperthyroidism. The drug does not inactivate existing thyroxine and triiodothyronine that are stored in the thyroid or circulating in the blood nor does it interfere with the effectiveness of thyroid hormones given by mouth or by injection. Methimazole is readily absorbed in the gastrointestinal tract, metabolized in the liver, and excreted in the urine.
Dosage & Administration
Methimazole is administered orally. The total daily dosage is usually given in 3 divided doses at approximately 8 hour intervals.
Adults: The initial daily dosage is 15 mg for mild hyperthyroidism, 30 to 40 mg for moderately severe hyperthyroidism, and 60 mg for severe hyperthyroidism, divided into 3 doses at 8 hour intervals. The maintenance dosage is 5 to 15 mg daily.
Pediatric: Initially, the daily dosage is 0.4 mg/kg of body weight divided into 3 doses and given at 8 hour intervals. The maintenance dosage is approximately 1/2 of the initial dose.
Use in children & adolescents: Because of post-marketing reports of severe liver injury in pediatric patient treated with propylthiouracil, Methimazole is the preferred choice when an antithyroid drug is required for a pediatric patient.
Adults: The initial daily dosage is 15 mg for mild hyperthyroidism, 30 to 40 mg for moderately severe hyperthyroidism, and 60 mg for severe hyperthyroidism, divided into 3 doses at 8 hour intervals. The maintenance dosage is 5 to 15 mg daily.
Pediatric: Initially, the daily dosage is 0.4 mg/kg of body weight divided into 3 doses and given at 8 hour intervals. The maintenance dosage is approximately 1/2 of the initial dose.
Use in children & adolescents: Because of post-marketing reports of severe liver injury in pediatric patient treated with propylthiouracil, Methimazole is the preferred choice when an antithyroid drug is required for a pediatric patient.
* রেজিস্টার্ড চিকিৎসকের পরামর্শ মোতাবেক ঔষধ সেবন করুন
Interaction
With medicine: Anticoagulants (oral)- Due to potential inhibition of vitamin K activity by Thyzol, the activity of oral anticoagulants (e.g., warfarin) may be increased; additional monitoring of PT/INR should be considered, especially before surgical procedures. β-adrenergic blocking agents- Hyperthyroidism may cause an increased clearance of beta-blockers with a high extraction ratio. A dose reduction of beta-adrenergic blockers may be needed when a hyperthyroid patient becomes euthyroid. Digitalis glycosides- Serum digitalis levels may be increased when hyperthyroid patients on a stable digitalis glycoside regimen become euthyroid; a reduced dosage of digitalis glycosides may be needed. Theophylline- Theophylline clearance may decrease when hyperthyroid patients on a stable theophylline regimen become euthyroid; a reduced dose of theophylline may be needed.
With food: Always take at the same moment in regard to meals, food may affect absorption unpredictably.
With food: Always take at the same moment in regard to meals, food may affect absorption unpredictably.
Contraindications
Methimazole is contraindicated in the presence of hypersensitivity to the drug or any of the other product components.
Side Effects
Common: Skin rash, urticaria, nausea, vomiting, epigastric distress, arthralgia, paresthesia, loss of taste, abnormal loss of hair, myalgia, headache, pruritus, drowsiness, neuritis, edema, vertigo, skin pigmentation, jaundice, sialadenopathy, and lymphadenopathy.
Rare: Agranulocytosis, granulocytopenia, thrombocytopenia and aplastic anemia, drug fever, a lupus-like syndrome, insulin autoimmune syndrome (which can result in hypoglycemic coma), hepatitis (jaundice may persist for several weeks after discontinuation of the drug), periarteritis, and hypoprothrombinemia. Nephritis occurs very rarely.
Rare: Agranulocytosis, granulocytopenia, thrombocytopenia and aplastic anemia, drug fever, a lupus-like syndrome, insulin autoimmune syndrome (which can result in hypoglycemic coma), hepatitis (jaundice may persist for several weeks after discontinuation of the drug), periarteritis, and hypoprothrombinemia. Nephritis occurs very rarely.
Pregnancy & Lactation
Pregnancy Category D. Due to the rare occurrence of congenital malformations associated with methimazole use, it may be appropriate to use other agents in pregnant women requiring treatment for hyperthyroidism particularly in the first trimester of pregnancy. Methimazole is excreted into breast milk. However, several studies found no effect on clinical status in nursing infants of mothers taking methimazole, particularly if thyroid function is monitored at frequent (weekly or biweekly) intervals.
Precautions & Warnings
Congenital Malformations: Thyzol readily crosses the placental membranes and can cause fetal harm, particularly when administered in the first trimester of pregnancy. If Thyzol is used during pregnancy or if the patient becomes pregnant while taking Thyzol, the patient should be warned of the potential hazard to the fetus. Since some congenital defects have been reported in offspring of patients treated with Thyzol, it may be appropriate to use other agents in pregnant women requiring treatment for hyperthyroidism, particularly in the first trimester of pregnancy. If Thyzol is used, the lowest possible dose to control the disease should be given.
Agranulocytosis: Agranulocytosis is potentially a life-threatening adverse reaction of Thyzol therapy. Patients should be instructed to immediately report to their physicians if any symptoms suggestive of agranulocytosis, such as fever or sore throat occur. Leukopenia, thrombocytopenia, and aplastic anemia (pancytopenia) may also occur. The drug should be discontinued in the presence of agranulocytosis, aplastic anemia (pancytopenia), ANCA-positive vasculitis, hepatitis, or exfoliative dermatitis and the patient’s bone marrow indices should be monitored.
Liver Toxicity: Although there have been reports of hepatotoxicity associated with Thyzol, the risk of hepatotoxicity appears to be less with Thyzol than with propylthiouracil, especially in the pediatric population. Drug treatment should be discontinued promptly in the event of clinically significant evidence of liver abnormality including hepatic transaminase values exceeding 3 times the upper limit of normal.
Hypothyroidism: Thyzol can cause hypothyroidism necessitating routine monitoring of TSH and free T4 levels with adjustments in dosing to maintain a euthyroid state. Because the drug readily crosses placental membranes, Thyzol can cause fetal goiter and cretinism when administered to a pregnant woman. For this reason, it is important that a sufficient, but not excessive, dose be given during pregnancy. Because Thyzol may cause hypoprothrombinemia and bleeding, prothrombin time should be monitored during therapy with the drug, especially before surgical procedures. Thyroid function tests should be monitored periodically during therapy. Once clinical evidence of hyperthyroidism has resolved, the finding of a rising serum TSH indicates that a lower maintenance dose of Thyzol should be employed.
Agranulocytosis: Agranulocytosis is potentially a life-threatening adverse reaction of Thyzol therapy. Patients should be instructed to immediately report to their physicians if any symptoms suggestive of agranulocytosis, such as fever or sore throat occur. Leukopenia, thrombocytopenia, and aplastic anemia (pancytopenia) may also occur. The drug should be discontinued in the presence of agranulocytosis, aplastic anemia (pancytopenia), ANCA-positive vasculitis, hepatitis, or exfoliative dermatitis and the patient’s bone marrow indices should be monitored.
Liver Toxicity: Although there have been reports of hepatotoxicity associated with Thyzol, the risk of hepatotoxicity appears to be less with Thyzol than with propylthiouracil, especially in the pediatric population. Drug treatment should be discontinued promptly in the event of clinically significant evidence of liver abnormality including hepatic transaminase values exceeding 3 times the upper limit of normal.
Hypothyroidism: Thyzol can cause hypothyroidism necessitating routine monitoring of TSH and free T4 levels with adjustments in dosing to maintain a euthyroid state. Because the drug readily crosses placental membranes, Thyzol can cause fetal goiter and cretinism when administered to a pregnant woman. For this reason, it is important that a sufficient, but not excessive, dose be given during pregnancy. Because Thyzol may cause hypoprothrombinemia and bleeding, prothrombin time should be monitored during therapy with the drug, especially before surgical procedures. Thyroid function tests should be monitored periodically during therapy. Once clinical evidence of hyperthyroidism has resolved, the finding of a rising serum TSH indicates that a lower maintenance dose of Thyzol should be employed.
Overdose Effects
Symptoms may include nausea, vomiting, epigastric distress, headache, fever, joint pain, pruritus, and edema. Aplastic anemia or agranulocytosis may be manifested in hours to days. Less frequent events are hepatitis, nephrotic syndrome, exfoliative dermatitis, neuropathies, and CNS stimulation or depression. In the event of an overdose, appropriate supportive treatment should be initiated as dictated by the patient’s medical status.
Therapeutic Class
Anti-thyroid drugs
Storage Conditions
Store in a cool (below 30°C) and dry place, away from light and children.
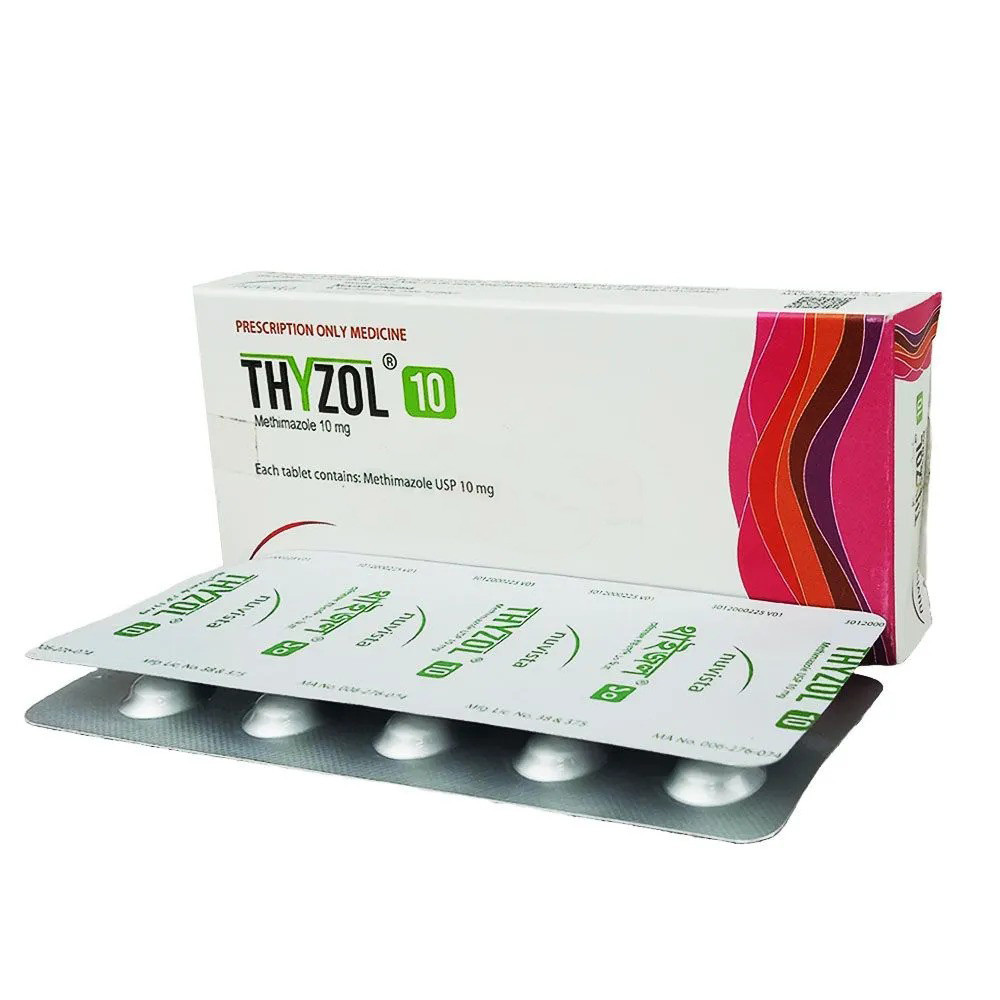
Pack Images: Thyzol 10 mg Tablet